Overview
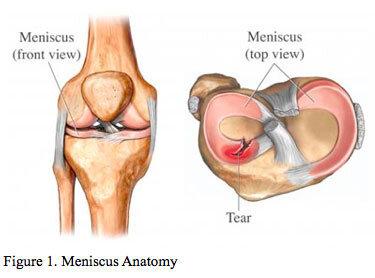
The meniscus is a C shaped piece of fibrous cartilage in the knee joint between the weight bearing surfaces of the femur and the tibia (Figure 1). There are two menisci in each knee, one on the inner side of the knee (medial meniscus) and one on the outer side of the knee (lateral meniscus).
The meniscus functions as a shock absorber for the knee, dissipating about a third of the force across the knee joint. It also acts as a stabilizer of the knee joint. The meniscus is a unique tissue in the body and only has blood vessels supplying its outermost portion. The inner portion of the meniscus receives its nutrients by diffusion alone. Because the blood supply to the meniscus is poor, tears of the meniscus usually do not heal on their own.
Meniscus Tears
Tears of the meniscus usually occur by two different mechanisms. A traumatic meniscal tear occurs when a patient recalls a specific twisting event during sports or a trauma to the knee. A degenerative meniscus tear is more subtle in onset with gradual development of symptoms in the inner or outer compartment of the knee. A traumatic tear can occur in a normal meniscus while a degenerative tear usually can occur because the quality of our meniscal tissue decreases with age. Meniscal tears are classified and treated based on their location within the knee, tear pattern, complexity of the tear, and quality of the tissue.
Symptoms
A patient with a meniscus tear will complain of knee pain and swelling on the inner (medial) or outer (lateral) side of the knee. There will be pain with deep knee bending, walking, twisting, and exercise. There can be a sensation of the knee giving way and mechanical symptoms such as locking, catching, or clicking.
Physical Examination
The physical examination is relatively reliable tool for the diagnosis of a meniscus tear. With a symptomatic meniscus tear, you will likely have swelling in your knee (effusion) and tenderness along the joint line when the doctor presses on the meniscus (palpation). In addition, loading the knee with specific maneuvers or a squat will cause pain in the compartment with the meniscus tear.
Imaging
- X-rays: X-rays are important in the diagnosis of knee injuries. These images are essential screening tools to rule out fracture in the setting of acute knee injuries and to rule out arthritis in chronic knee pain. In the setting of a chronic knee condition the x-rays show the amount of joint space (cartilage) left in the knee.
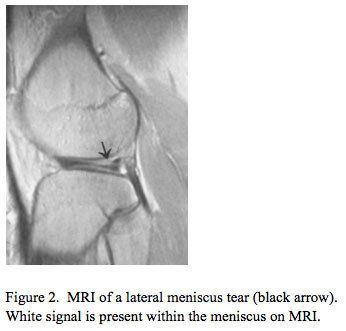
- MRI: MRI (magnetic resonance imaging) has become an essential tool for knee surgeons. While x-rays are excellent at showing bony anatomy, arthritis, and fractures, MRI is very sensitive for detecting injuries to the soft tissues of the knee including cartilage, meniscus, and ligament. Meniscus is shown on an MRI as a series of slices that resemble black triangles. Meniscal tears are seen on MRI as an area of white signal (tearing) through the meniscus tissue (Figure 2).
Treatment - Knee Arthroscopy
Because of the poor healing capacity of the meniscus, most symptomatic meniscus tears caused by trauma require arthroscopic surgical treatment to repair the meniscus or remove the torn piece of meniscus.
A degenerative tear is often given a chance to improve with time. Initial treatment is with R.I.C.E. (rest, ice, compression, and elevation), anti-inflammatories, and physical therapy for a period of 4-6 weeks prior to making a decision for surgery.
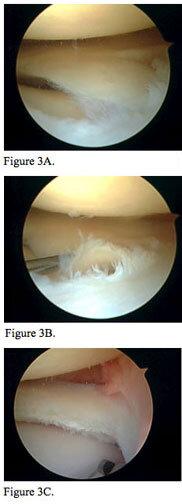
At the time of surgery, your surgeon will make a determination of whether or not the meniscus tear is repairable. Complex tears and degenerative tears are usually not amenable to repair and are treated with arthroscopic partial meniscectomy (Figure 3). All efforts are made to preserve as much meniscus as possible.
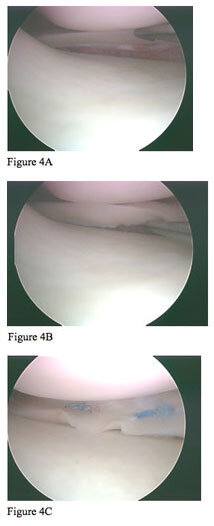
Generally, meniscus tears that are traumatic in nature, longitudinal, and near the outside (periphery) of the knee are amenable to repair. These tears are treated with arthroscopic meniscal repair (Figure 4). Smaller tears can be repaired without making a separate incision via an all inside technique. Dr. Gamradt uses the Fast-fix from Smith and Nephew. This system allows the repair of many smaller meniscal tears with excellent results in a minimally invasive fashion.
Figure 3. Arthroscopic partial meniscectomy. Arthroscopic pictures of a traumatic, complex lateral meniscus flap tear (3A, 3B) that was treated with partial meniscectomy. Notice the preserve rim of good meniscal tissue present after removal of the torn tissue (3C).
Figure 4. Arthroscopic pictures of a traumatic, simple, longitudinal tear in the area of the meniscus with blood supply (peripheral) (4A, 4B). This meniscus tear was repaired using an all-inside technique with the Fast-fix meniscal repair system. Notice the blue sutures holding the repaired tear in place (4C).
What to Expect
Pre-Op
- X-rays and an MRI of your knee will be ordered to aid in preoperative planning and diagnosis.
- If you have any medical problems or are over the age of 50, you will need a consultation with your PMD and/or cardiologist prior to surgery to ensure that you are safe for anesthesia. Your doctor may order lab tests and an EKG.
Day of Surgery
- Outpatient surgery-you will come in and go Seth C. Gamradt, MD, Orthopedic Surgeon, Beverly Hills, Los Angeles, CA the same day.
- Nothing to eat or drink past midnight the night before surgery
- Surgery lasts 1-1½ hours depending on the type of meniscus tear.
- Surgery can be performed under three types of anesthesia depending on your preference. You can decide the day of surgery after discussing this with your anesthesiologist.
- Local with sedation
- Spinal anesthesia
- General
- Your knee will be in an Ace bandage postoperatively and this bandage can be changed on post-op day 2.
- You will use crutches for 3-7 days. Bearing weight on the leg is safe.
Post-Op/Rehab
Partial meniscectomy: In 5-7 days, you will likely be walking comfortably. You will perform a Seth C. Gamradt, MD, Orthopedic Surgeon, Beverly Hills, Los Angeles, CA exercise program daily for the first 10 days. At the first visit, Dr. Gamradt will decide whether you need formal physical therapy or a continuation of the Seth C. Gamradt, MD, Orthopedic Surgeon, Beverly Hills, Los Angeles, CA exercise program.
- Post-op visits:
- 10-14 days: suture removal, check motion, get physical therapy prescription.
- 6 weeks: range of motion check, return to sport/activity
- 12 weeks: final checkup.
Meniscal Repair: Meniscal repair rehabilitation is longer than a partial meniscectomy as the meniscus requires time to heal. You will be in a brace for six weeks after surgery and motion will be limited to 90 degrees of flexion for this period. Weight bearing will be allowed with the brace locked only.
- Post-op visits:
- 10-14 days: suture removal, check motion, get physical therapy prescription.
- 6 weeks: Remove brace, range of motion check.
- 12 weeks: return to sport/activity






