Overview
Dr. Gamradt has a special interest in the nonoperative and operative treatment of shoulder fractures. These fractures usually occur in the young during high energy falls and accidents. These fractures can also occur in the elderly due to less severe trauma such as a ground level fall. Many fractures can be treated with immobilization and rehabilitation without surgery. Certain severe fractures require surgery to restore shoulder function.
Proximal Humerus Fractures
In some circumstances, the proximal humerus is so badly damaged that fixation with a locking plate is not feasible. In these circumstances, the fractures are treated with a hemiarthroplasty or a reverse arthroplasty.
A hemiarthroplasty is a partial shoulder replacement that replaces the damaged head of the humerus with a metal ball affixed to a stem inserted in the humeral shaft. The hemiarthroplasty used is specifically designed for treatment of fractures and has a specialized shape and coating to allow for healing of bone to metal. The rotator cuff muscles and their attachments to bone (tuberosities) are securely fixed to the prosthesis using heavy suture or wire.
A reverse arthroplasty is reserved of especially bad fractures with severe fragmentation of the shoulder. A ball is inserted onto the shoulder socket and a socket is inserted into the humerus. The rotator cuff muscles and their attachments to bone (tuberosities) are securely fixed to the prosthesis using heavy suture or wire.
In many centers reverse arthroplasty is gradually replacing hemiarthroplasty as the shoulder replacement of choice in severe proximal humerus fractures due to increased predictability of the result, especially in elderly patients.
Surgery is performed as an inpatient. Hospital stay is 1-2 nights.
After surgery, the arm is held in a sling for six weeks. Gentle protected range of motion begins immediately after surgery in most cases. Rehabilitation continues for 3-6 months after surgery. Again, due to the complex function and mobility of the shoulder, range of motion and strength do not normalize after surgery but the shoulder usually has minimal pain when healing is complete.
Non-Operative Treatment
When a fracture is minimally displaced, alignment of the bone is close to normal, and nonoperative treatment of the fracture can result in excellent functional outcomes. A brief period of immobilization (1-3 weeks) in a sling is followed by gentle passive motion. When the fracture is healed on x-ray, more aggressive range of motion and strengthening begins with the guidance of a physical therapist. The following x-ray is an example of a fracture that can be successfully treated non-operatively. Because the shoulder joint has more motion than any joint in the body, even an innocuous appearing fracture can cause a permanent loss of motion. Figure 1 shows a non-displaced proximal humerus fracture that can be successfully treated non-operatively.
Figure 1. Non-displaced fracture of the proximal humerus. The humerus is fractured, but retains normal shape and alignment. A brief period of immobilization and physical therapy can result in a successful outcome.
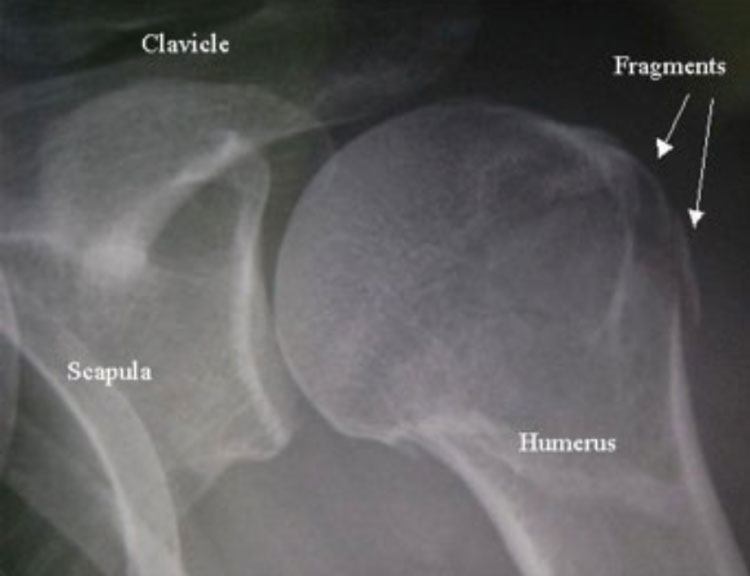
Figure 1.
Surgical Treatment of Proximal Humerus Fractures: Open Reduction and Internal Fixation (ORIF)
With increasing displacement of fracture fragments, the likelihood of a successful result without surgery decreases. With displacement, the humerus loses its shape and does not rotate normally within the socket (glenoid). In addition, the attachment of the rotator cuff muscles to the proximal humerus is often compromised. In this setting, surgery is often recommended to restore normal proximal humeral anatomy and give the best chance at function. Surgery is performed 1-3 weeks after injury; this is after peak swelling has occurred, but before the fracture has begun to heal in the abnormal position.
Surgery is performed under general anesthesia usually with regional anesthesia as well (nerve block). A four-inch incision is made over the front of the shoulder and a specialized plate and screws are inserted that are specifically designed for the proximal humerus. This plate and screws holds the fracture in anatomic alignment while it heals. Hospital stay is 1-2 nights. A sling is worn for 4-6 weeks. Physical therapy is then performed for 3-4 months. Range of motion and strength will continue to improve throughout the first year after the fracture. Due to the complex nature of the shoulder and the high degree of mobility required for normal function, some range of motion and strength deficits can persist permanently. Figure 2 shows the proximal humeral locking plate and two fractures successfully treated with open reduction and internal fixation.
Figure 2 (A-E). 2A. Proximal humeral locking plate
2B and 2D. Displaced proximal humerus fractures before fixation
2C and 2E. Proximal humerus fractures after open reduction and internal fixation with a locking plate.
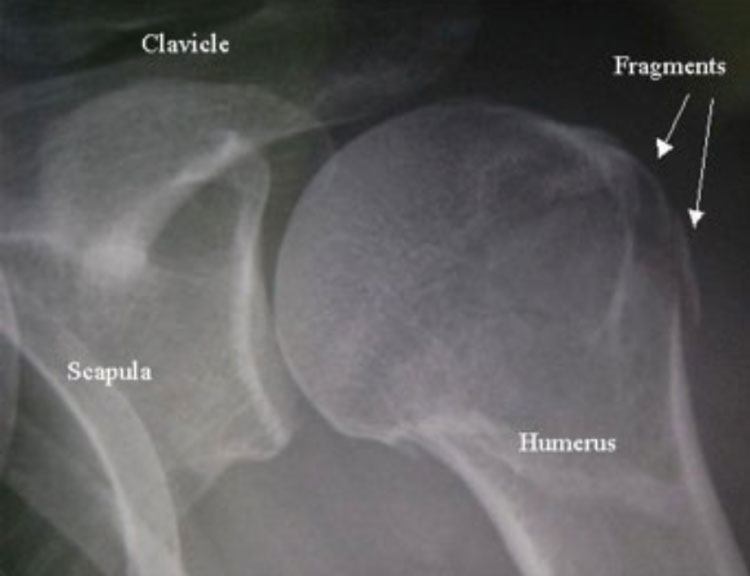
Figure 2
Proximal Humerus Fractures Treated with Hemiarthroplasty
In some circumstances, the proximal humerus is so badly damaged that fixation with a locking plate is not feasible. In these circumstances, the fractures are treated with a hemiarthroplasty. A hemiarthroplasty is a partial shoulder replacement that replaces the damaged head of the humerus with a metal ball affixed to a stem inserted in the humeral shaft. The hemiarthroplasty used is specifically designed for treatment of fractures and has a specialized shape and coating to allow for healing of bone to metal. The rotator cuff muscles and their attachments to bone (tuberosities) are securely fixed to the prosthesis using heavy suture or wire. Surgery is performed as an inpatient. Hospital stay is 2 nights.
After surgery, the arm is held in a sling for six weeks. Gentle protected range of motion begins immediately after surgery in most cases. Rehabilitation continues for 3-6 months after surgery. Again, due to the complex function and mobility of the shoulder, range of motion and strength do not normalize after surgery but the shoulder usually has minimal pain when healing is complete. Figure 3 shows a severe proximal humerus fracture treated with hemiarthroplasty.
Figure 3A: Fracture specific shoulder hemiarthroplasty. 3B: Severely comminuted proximal humerus fracture. 3C: Fracture after treatment with fracture specific hemiarthroplasty shoulder alignment is restored.
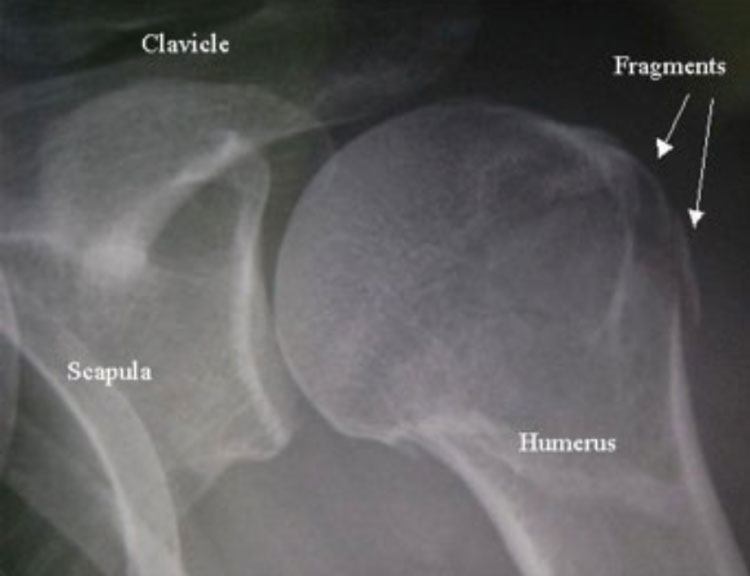
Figure 3
Clavicle Fractures
The clavicle is an S-shaped bone that serves as an attachment for many muscles and as a strut from the sternum to the acromion (scapula). The clavicle is frequently fractured in falls, sports, or higher energy injuries such as car accidents. Most clavicle fractures can be treated non-surgically with a period of immobilization in a sling or clavicle strap followed by gradual return to activity as the bone heals over the course of the next 6-8 weeks. Figure 4 shows a nondisplaced clavicle fracture that will heal with essentially no insult to shoulder function without surgery.

Figure 4A

Figure 4B

Figure 5A
Figure 5A. Nondisplaced clavicle fracture
Some clavicle fractures are sustained with a higher degree of energy and result in severe displacement. The displacement of the fracture results in a predictable pattern of deformity in the shoulder. First, the fracture fragments tend to over-ride one another so that there is shortening of the clavicle due to unrestricted pull of musculature crossing the fracture site. Second, the weight of the arm tends to pull the lateral fragment inferiorly with respect to the medial fragment which is held superiorly by the pull of the trapezius muscle. Traditionally, this deformity off the clavicle was accepted as long as the fracture fragments did not threaten the overlying skin. However, a landmark study that involved randomization of patients with displaced clavicle fractures into surgical and nonsurgical treatment showed that surgery more predictably returned patients back to normal shoulder function. For this reason, many shoulder surgeons have begun treating clavicle fractures with a high degree of displacement with surgery. A second type of clavicle fracture that is commonly treated with surgery is a distal clavicle fracture. Distal implies that the fracture has occurred near the outer edge of the clavicle. This type of fracture also predictably results in a high degree of displacement and deformity and can require surgery.
Surgery is performed by making and incision over the clavicle and inserting a specially contoured plate designed to fit the specific side (right or left) and length of the patient’s clavicle. The plate is affixed to the bone with specialized locking screws. This construct holds the fracture in anatomic alignment until the fracture heals. Surgical treatment does carry a risk of scar formation, infection, nonunion, and wound healing problems. These problems occur very rarely and the risks have proven to be acceptable when trying to avoid permanent deformity to the shoulder caused by a highly displaced clavicle fracture. After surgery, the patient can choose to go Seth C. Gamradt, MD, Orthopedic Surgeon, Beverly Hills, Los Angeles, CA after surgery or remain in the hospital one night. A sling is required for 4 weeks. Range of motion and strengthening exercises usually return the shoulder to close to normal function after 3-4 months. Figure 4 shows a highly displaced midshaft clavicle fracture and highly displaced distal clavicle fracture treated with surgery.
Figure 5B: Clavicle specific locking plates. 4C-D. Displaced midshaft clavicle fracture before and after treatment with a locking clavicle plate. 4D-E. Displaced distal clavicle fracture before and after treatment with a locking hook plate (F) or a locking precontoured distal clavicle plate (G).
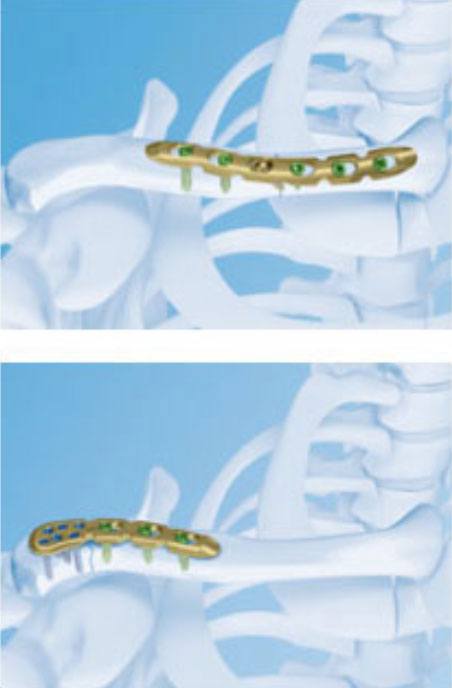
Figure 5B

Figure 5 C-G
Glenoid Fractures
The glenoid forms the socket of the ball and socket joint of the shoulder. Traumatic injuries to the shoulder can sometimes result in fractures to the glenoid. If the glenoid fracture fragment is large enough it can compromise the joint surface or the stability of the shoulder joint. In some cases, this fracture can be repaired arthroscopically. In others (Figure 5), the fracture is treated with screw fixation. Surgery and rehabilitation is similar to rehabilitation of a proximal humerus fracture.
Figure 6: Glenoid fracture involving 35% of the articular surface compromising stability of the shoulder. Fracture before (A) and after (B) fixation with 2 screws.

Figure 6A

Figure 6B











