Overview
Shoulder replacement is a treatment for end stage arthritis of the shoulder joint. If a patient has failed nonoperative treatment, (physical therapy, medications, injections, rest), shoulder replacement becomes a surgical alternative to relieve pain. The procedure involves replacing the shoulder joint with metal and plastic to alleviate the pain from bone on bone arthritis and improve function.
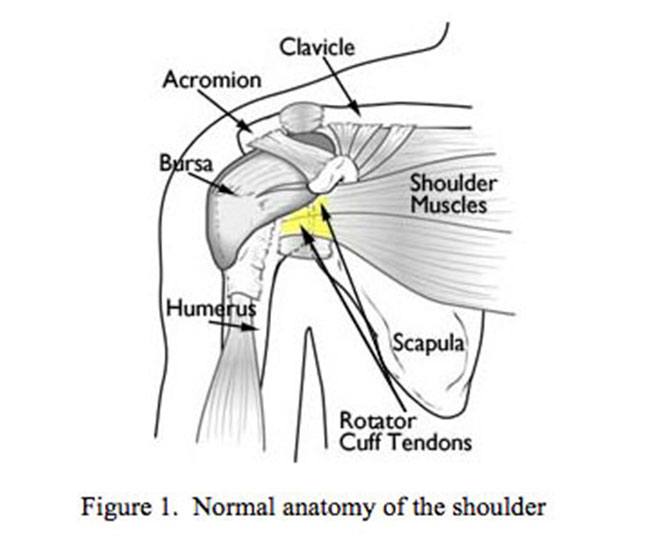
Figure 1. Normal anatomy of the shoulder
Symptoms
The normal shoulder is a ball and socket joint (Figure 1). The ball is called the humeral head and the socket is called the glenoid. In shoulder arthritis, the cartilage (gliding surface for the joint) is destroyed by wear and tear, inflammation, previous injury, or failed previous shoulder surgery. The hallmarks of shoulder arthritis are chronic pain exacerbated by shoulder activity and limited range of motion. In addition, there is difficulty sleeping on the affected shoulder and an inability to perform simple tasks without pain.
Treatment
Initial treatment for shoulder arthritis should include the following conservative treatment measures:
- Rest: Because the shoulder is not a weight bearing joint like the knee, simply modifying one’s activities can improve symptoms
- Medications: Tylenol or anti-inflammatories can help with symptoms
- Injections: Steroid injections or visco-supplementation (e.g. Synvisc) can provide temporary relief.
- Physical therapy: Range of motion exercises and strengthening can improve symptoms.
- Arthroscopy: In less severe cases of arthritis, removal of spurs and loose cartilage can provide temporary relief of symptoms. Arthroscopy is typically ineffective in severe arthritis.
Types of Shoulder Arthritis
Shoulder arthritis has several different causes
- Osteoarthritis: Degenerative joint disease
- Rheumatoid arthritis or other inflammatory arthritis
- Arthritis after previous shoulder instability surgery or multiple dislocations
- Avascular necrosis: lack of blood supply to humeral head causing collapse of the bone
- Cuff tear arthropathy: Arthritis caused by massive rotator cuff tear. This type of arthritis is usually treated with a special type of prosthesis called a reverse shoulder prosthesis.
Each type of shoulder arthritis has specific features that are unique that affect planning of surgery and the type of shoulder replacement needed. Based on physical examination, x-ray, and MRI or CT scan, your doctor will usually know what type of arthritis you have and whether or not you are a candidate for a shoulder replacement.

Figure 2A

Figure 2B
Figure 2. Normal shoulder AP (A.) and Axillary (B.) x-rays
Figure 3. AP (A.) and Axillary (B.) x-rays of an arthritic shoulder with joint space narrowing, bone spurs, and loose bodies. This shoulder has normal rotator cuff tendons and therefore preservation of the acromiohumeral distance.
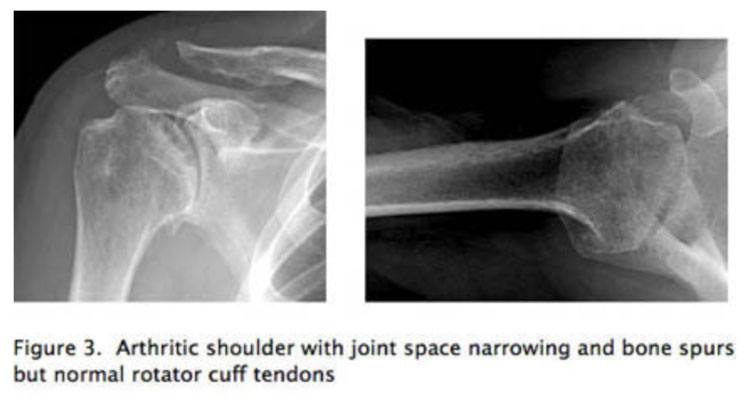
Figure 1. Normal anatomy of the shoulder
Shoulder Replacement
A normal shoulder has cartilage on the ball and socket to enable smooth gliding motion (Figure 2). In the arthritic shoulder the normal cartilage is worn away instead of cartilage gliding smoothly on cartilage, bone rubs roughly against bone, creating pain and inflammation. A shoulder replacement consists of a metal stem and ball that resurfaces the arthritic humerus bone (ball) and a plastic component that resurfaces the arthritic glenoid (socket), (Figure 3).
In a patient with arthritis, shoulder x-rays show joint space narrowing and osteophyte formation (bone spurs) (Figure 4). When the rotator cuff is intact and bone stock is good, a conventional shoulder replacement replaces the ball and socket joint with metal and plastic, eliminating pain and restoring range of motion (Figure 5).

Figure 4A

Figure 4B
Figure 4. These three x-rays represent a conventional shoulder replacement that is used when the rotator cuff is intact. Conventional shoulder replacement uses a press fit humeral stem and a cemented three pegged polyethylene glenoid component to resurface the shoulder joint and eliminate pain.
Figure 5A
Figure 5. Sometimes, the degenerative problem with the shoulder exists only on the humeral side of the shoulder joint. In this case, only the humerus is resurfaced using a conventional stemmed component or a resurfacing component. Figure 5A and 5B are preoperative x-rays of a patient with avascular necrosis of the humeral head with extensive involvement of the humeral head. In this condition, the bone has sustained a vascular insult resulting in dead bone that eventually collapses. In figure 5C, the shoulder has been replaced with a hemiarthroplasty.
In Figure 5B, the patient has evidence of post traumatic arthritis with extensive bone spur formation. In Figure 5C, the bone spurs have been removed and the humeral head has been resurfaced with a cap-type resurfacing prosthesis.

Figure 5B

Figure 5C
What to Expect
Pre-op
- A CAT scan and/or MRI of your shoulder will be ordered to aid in preoperative planning. These studies aid in assessing two important factors: rotator cuff tendons and bone available for the replacement.
- You will need a consultation with your PMD and/or cardiologist prior to surgery to ensure that you are safe for anesthesia.
- If you have had previous surgery, an infection workup will be performed, even if there is no sign of active infection: This will likely include an aspiration of the shoulder, lab work, and other tests.
Day of Surgery/Hospital Stay
- Nothing to eat or drink past midnight the night before surgery.
- Surgery lasts 2-3 hours depending on complexity.
- Surgery is performed under general anesthesia with a nerve block of the shoulder as well.
- Your arm will be in a sling postoperatively for 6 weeks.
- You will start exercises the day following surgery to move the shoulder passively.
- You will have a button to push to control your pain after surgery.
- You will have a small drain in your shoulder for 24-48 hours.
- You will stay on prophylactic antibiotics for 24 hours.
- You will likely have a Foley catheter in your bladder until the first day after the operation.
- Hospital stay is generally 2 nights.
- Blood transfusion is rarely needed except in revision surgery.
- You may need help at Seth C. Gamradt, MD, Orthopedic Surgeon, Beverly Hills, Los Angeles, CA to assist in daily living activities.
- For elderly patients who live alone we can arrange inpatient rehabilitation.
Post-Op/Rehab
- Post-op visits:
- 2 weeks: suture removal, x-ray, check motion ensure proper performance of Seth C. Gamradt, MD, Orthopedic Surgeon, Beverly Hills, Los Angeles, CA exercises.
- 6 weeks: Discontinue Sling. Start physical therapy
- 12 weeks: range of motion check, start strengthening.
- 24 weeks: X-ray, range of motion check.
- One year and yearly thereafter for x-rays.
- Your arm will be in a sling 6 weeks.
- Sutures come out at 1-2 weeks postop. The wound should be kept dry until then. After sutures come out, normal showering can begin.
- Supervised physical therapy starts at week 6 and continues for three months. No strengthening until 12 weeks post-surgery.
- Final healing 6 months or more.
- Dental prophylaxis: Amoxicillin (2 grams one hour prior to procedure). If you have a penicillin allergy you should take Clindamycin (600 mg one hour prior to procedure).
Complications
The complication rate for shoulder replacement is low. However, as with any joint replacement, the pain and disability must be significant enough to warrant surgery. Complications can include:
- Infection
- Stiffness of shoulder
- Continued pain
- Fracture of humerus or glenoid
- Nerve injury
- Loosening requiring revision surgery
- Medical complications (stroke, heart attack, pulmonary embolus)
Do I Have to Undergo a Shoulder Replacement?
Shoulder replacement is for severe pain and shoulder functional limitations that affect daily life. Prior to undergoing a shoulder replacement, you should have tried physical therapy, injections, medications, activity modification and watchful waiting, all without improvement. Only you can decide when the right time for a shoulder replacement has arrived.
Although there are risks of shoulder replacement surgery, results are generally excellent in the properly selected patient with sufficient bone stock and an intact rotator cuff.











